Abstract
Introduction
Chronic deep venous insufficiency (CVI) is a common disorder of the venous valves which can cause many debilitating symptoms including edema, pain, and skin changes. CVI may result from a primary non-thrombotic cause, such as May-Thurner syndrome (MTS) or extrinsic compression from a pelvic mass, or as the sequelae of an acute deep vein thrombosis (DVT). Endovascular interventions, including percutaneous transluminal angioplasty and venous stent placement, have been increasingly utilized as a minimally-invasive treatment option for CVI. In patients treated via endovascular therapy, stent restenosis is a significant area of clinical concern. However, there is a paucity of data on the optimal preventative long-term antithrombotic strategy. Current practice is highly variable and employs a combination of anticoagulation and antiplatelet agents, which borrows heavily from experience with venous thromboembolism and arterial stent management, respectively. This study examines the prescribing patterns and outcomes of various antithrombotic regimens after venous stent placement at a large academic medical center.
Methods
Patients who received venous stents at our institution between January 1st, 2010 and December 31st, 2015 were eligible for the study. A retrospective review was performed to determine the antithrombotic regimens and the rates of stent restenosis and major bleeding within two years of stent placement. The relationship between these outcomes and antithrombotic regimens was analyzed via logistic regression. Additional logistic regression and linear regression models were used to evaluate the impact of indications and hypercoagulable risk factors on the selection of antithrombotic agents.
Results
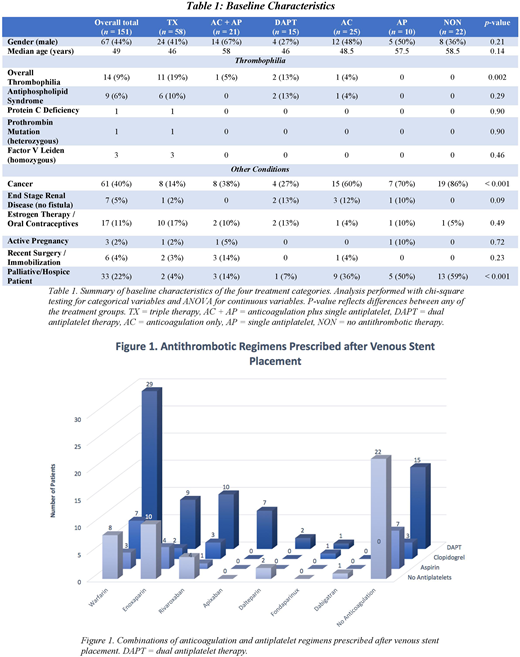
A total of 151 patients were included in the study (Table 1). Antithrombotic regimens were variable: 58 patients (38%) received triple therapy (i.e., anticoagulation plus dual antiplatelet therapy), 25 (17%) received anticoagulation only, 21 (14%) received anticoagulation plus a single antiplatelet agent, 15 (10%) received dual antiplatelet therapy only, 10 (7%) received a single antiplatelet, and 22 (15%) received no antithrombotic therapy (Figure 1). Patients with acute DVTs with or without MTS were more frequently given multiple antithrombotic agents compared to those with extrinsic compression. The duration of antithrombotic therapy was also variable. When anticoagulation was prescribed (n = 104), 31% received indefinite therapy, followed by 22% for 6 months and 12% for 3 months. Patients with a history of prior DVTs or thrombophilia were more likely to be prescribed indefinite anticoagulation. Aspirin was most commonly prescribed for an indefinite duration (62 of 88 patients) while clopidogrel was most commonly prescribed for just 3 months (60 of 89 patients).
Twenty-three patients (15%) developed stent restenosis. Triple antithrombotic therapy had significantly lower rates of stent restenosis compared to no antithrombotic therapy (OR = 0.05, p < 0.01), and was associated with lower rates of restenosis compared to anticoagulation alone (OR = 0.19, p = 0.07) and dual antiplatelet therapy (OR = 0.25, p = 0.09). Anticoagulation with a single antiplatelet agent also led to lower rates of stent restenosis when compared to no antithrombotic therapy (OR = 0.08, p = 0.04). Medication non-compliance and antiphospholipid antibody syndrome were identified as independent predictors of stent restenosis (OR = 8.84, p = 0.01 and OR = 7.11, p = 0.03, respectively). Major bleeding was observed in 11 patients (7%). Of note, there were no major bleeding events observed in the dual antiplatelet or single antiplatelet groups, which were thus excluded from the regression model. Among the remaining treatment groups, there was no significant difference in major bleeding rates.
Conclusions
This study emphasizes the considerable variability in the prescribing patterns of long-term antithrombotic therapy after venous stent placement. There appears to be benefit to antithrombotic therapy in preventing stent restenosis, particularly when anticoagulation is combined with antiplatelet agents. However, this may be counterbalanced by an increased risk of bleeding. Larger prospective trials are needed to evaluate the relative risks and benefits of each antithrombotic regimen, and ultimately determine the optimal management strategy, following venous stent placement.
Desai:Philips/Spectranetics: Other: consulting; Cook Medical: Other: consulting, Speakers Bureau; Boston Scientific: Other: consulting, Speakers Bureau; AngioDynamics: Other: consulting, Speakers Bureau; OptiMed: Other: consulting.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal